Schedule Appointment

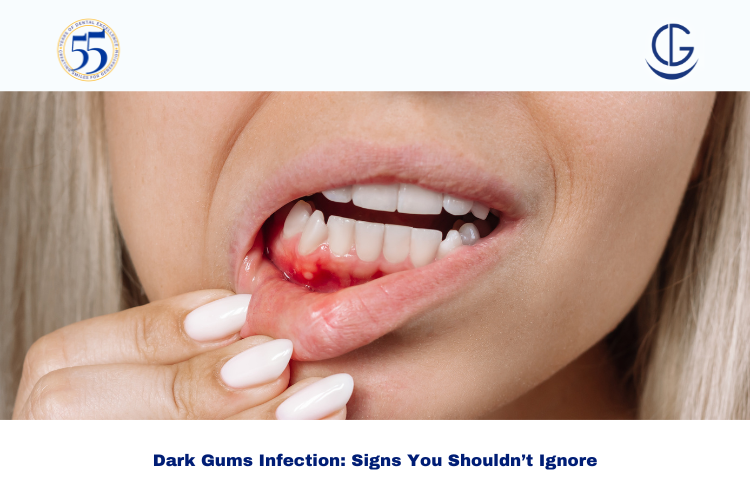
Dark gums infection is more than a cosmetic concern. In many cases, it’s your mouth’s early warning signal that inflammation, bacterial buildup, or gum disease may be developing under the surface. If you’ve noticed your gums turning darker around one tooth, along the gumline, or across the mouth, it’s worth checking what’s normal pigmentation and what could be a treatable infection.
At Dr Gowds Dental Hospitals, we regularly see patients across Hyderabad who delay care because “it doesn’t hurt much” or they assume dark gums are permanent. The truth is: some causes are harmless, but others need timely treatment to protect your gums, teeth, and overall oral comfort.
If you’re seeing dark gums, bleeding, swelling, or bad breath, book a consultation at Dr Gowds Dental Hospitals.
Not all dark gums are a problem. Some people naturally have deeper gum pigmentation due to melanin, similar to skin tone variation. This is common and usually symmetrical across the mouth.
However, darkening that appears suddenly, becomes patchy, or is paired with discomfort may indicate infection or inflammation.
If you notice these changes, it’s smart to evaluate for gum infection symptoms rather than assuming it’s purely cosmetic.
A “dark gums infection” typically refers to gum tissue that looks darker because of:
In Hyderabad, this is especially common in people dealing with:
Dark gums may be one visible change, but infection often comes with additional signals. Here are common gum infection symptoms patients report:
If you have serious symptoms, don’t self-treat at home. Seek a dental evaluation quickly.
Gingivitis is inflammation caused by plaque buildup. It can make gums look darker, swollen, and prone to bleeding. The good news: it’s often reversible with professional cleaning and consistent home care.
When gum infection goes deeper, it can damage the bone supporting your teeth. Gums may appear dark red, purple, or brownish—especially near pockets where bacteria are trapped.
Even if teeth look “clean,” hardened tartar under the gum can trigger ongoing inflammation. This is common in patients who brush regularly but haven’t had professional cleaning in a long time.
Tobacco reduces blood supply to gums and increases pigmentation. It can also mask bleeding, meaning the disease progresses quietly while gums darken.
Margins that trap food can cause chronic irritation. If you see dark gum tissue around a crown, bridge, or old filling, it may be an infection risk.
Pregnancy, diabetes, and certain medications can increase gum inflammation. If you’re noticing changes along with frequent swelling or bleeding, a dental exam helps rule out infection.
Ignoring dark gums when infection is involved can lead to:
A simple gum check in a trusted clinic can prevent months (or years) of discomfort.
A professional gum evaluation typically includes:
For plaque/tartar-driven inflammation, scaling removes deposits that brushing can’t reach.
If gum pockets have formed, deep cleaning removes bacteria from below the gumline and smoothens root surfaces to help gums reattach.
If there’s active infection, your dentist may recommend topical or oral medication based on clinical findings. Not every gum problem needs antibiotics—proper cleaning often resolves most cases.
For persistent pockets or severe periodontitis, periodontal treatment may be recommended to control infection and protect bone support.
In some patients, crowding or bite imbalance traps plaque or increases gum strain. If this contributes to recurring inflammation, you can talk to an orthodontist about whether braces or aligner treatment would reduce long-term gum stress and improve cleaning access.
These steps don’t replace a dental visit, but they can support recovery:
If bleeding increases or pain worsens, stop experimenting with home remedies and get evaluated.
Many Hyderabad patients work long hours, commute heavily, and rely on quick meals and frequent tea/coffee—habits that can quietly increase plaque retention. Add stress, irregular sleep, and delayed dental checkups, and gum inflammation can build over time without major pain.
If you’re noticing dark gums and any gum infection symptoms, it’s worth taking action early—especially before an important event, travel, or a busy work cycle where pain can suddenly spike.
If you’re noticing dark gums infection signs or other gum infection symptoms, don’t wait for it to become painful. Book a consultation at Dr Gowds Dental Hospitals and visit your nearest branch in Gachibowli, Madhapur, Koti, Nanakramguda. You can also talk to an orthodontist if crowding or bite issues may be contributing—and explore aligner treatment for a cleaner, healthier long-term smile.
Yes. Gum infections often progress with mild or no pain at first. Bleeding, swelling, or persistent bad breath alongside dark gums can still indicate inflammation.
Bleeding while brushing, swollen gums, pus near the gumline, bad breath that returns quickly, and pain while chewing are common warning signs.
If the cause is plaque/tartar-related inflammation (gingivitis), professional cleaning can significantly improve gum health. If it’s advanced disease, deep cleaning or periodontal care may be needed.
Mild cases may improve within 1–2 weeks after cleaning with proper home care. Deeper infections can take longer and may require multiple visits and follow-ups.
In some cases, yes. If crowding makes cleaning difficult or bite issues cause repeated gum irritation, orthodontic evaluation and aligner treatment can improve access for hygiene and reduce recurrence risk.